|
Home > Lungs and Respiratory Health Guide The Complete Guide to Your Lungs and Respiratory Health |
 |
Contents of the Complete Guide to Your Lungs
Your Lungs: Living Air Purifier Filters Within
Image of Red Blood Cell Heme Group
Image of Inhallation Hazards
Asbestos-related Disease Care Guide
- What is Asbestos?
- Image of Asbestos Fibers
- Asbestos Related Illnesses
- Image of Mesothelioma Cells
- Signs and Symptoms of Asbestosis
- Image of Asbestos Damaged Tissue
- Respiratory System Parts
- Image of Respiratory System
- Image of Alveoli Air Sacs
- Amazing Facts About Respiratory System
- Asbestos Breakdown Process
- Treatment of Asbestos-related Illnesses
- Respiratory Infections
- Steps to Prevent Infection
- Self-Care Tips for Managing Asbestos-related Disease
Learn More About Asbestos
Other Forms of Respiratory Disease
Effects of Air Pollutants
Toxic Air Pollutants
- Dust / Particulate Matter (PM)
- Image of What Happens When Dust is Inhaled
- What Happens When Dust is Inhaled
- Nitrogen Oxides (NOx) / Nitrogen Dioxide (NO2)
- Carbon Monoxide (CO)
- Ozone (O3)
- Sulfur Dioxide (SO2)
- Lead (Pb)
- Endotoxins
Contact the Home Air Purifier Expert
Your Lungs: Living Air Purifier Filters Within
 |
Think of your lungs as being a remarkably complex bio-mechanical air exchanger or living air purifier.
Like the chemical vapor absorbing materials found in the best air purifiers (such as activated carbon) your lungs are "designed" or "evolved" (which ever you prefer to believe) to filter out the smallest of gas particles; in fact, your life depends on your lungs' capacity to efficiently extract the tiniest of gaseous molecules of diatomic oxygen from air and they do it about 15 to 25 times per minute without any conscious direction on our part.
The respiratory system is itimately associated with the circulatory system such that over 9,000 liters of air meets with 10,000 liters of blood in the lungs every day. That blood is pumped by the heart to the lungs via the pulmonary artery.
The oxygen molecules from the inhaled air diffuse into the tiny capillaries which pass between and around the millions of air sacs or Alveoli inside the lungs. It has been estimated that if laid end to end the capillaries in the lungs would stretch for almost 1,000 miles.
For the most efficient gaseous exchange within the lungs the internal surface area of the lungs is estimated to exceed that of a tennis court. Most of this surface area is from these millions of Alveoli. The Aleveoli share the same very thin cell walls as the capillaries so oxygen does not have far to go before it enters the blood.
Likewise, poisonous carbon dioxide gas created by metabolic processes throughout the body easily diffuses out of the blood and is exhaled from the lungs.
As oxygen enters the capillaries it is bound by Hemoglobin which is an iron-containing metallo-protein found in the Red Blood Cells.
At any given moment we have about 30,000,000,000,000 (that's 30 TRILLION!) Red Blood Cells circulating throughout our body, and they contain a total of about 3.5 grams of Fe, almost five times the total amount found in other cell matter. The iron atoms at the center of the Heme units in Hemoglobin is the reason why Hemoglobin can bind and transport oxygen.
The oxygen carrying Red Blood Cells are then pumped back to the heart via the pulmonary vein and then circulated back to the cells throughout the body. When Red Blood Cells travel through capillaries in cells such as muscle cells, they unload their oxygen to be used for metabolic processes like cellular respiration.
The rate at which the lungs exchange life giving oxygen for the poisonous carbon dioxide made by our cells is automaticly regulated by the autonomic nervous system which gets feedback and regulates breathing according to our physical activity or ambient oxygen concentration.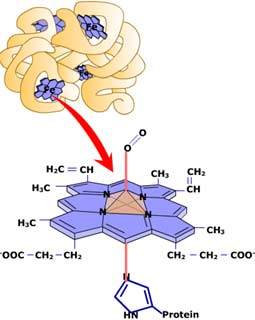
Because of this control system, breathing is not an action we can consciously cease to perform for very long.
So strong is the automatic reflex in control of our lungs' function, that we would only be able to willingly hold our breath for so long before our conscious will would be overridden by the autonomic will to increase breathing in responce to falling oxygen concentrations in the blood.
However, the proper functioning of the lungs is important to the body for not just gas exchange. The lungs also function to regulate the percent of hydrogen ions (or pH) of the blood. Your lungs are also important for filtering out small blood clots in the veins. Also, the lungs' spongy texture makes them an important protective cushion for the heart.
Clearly the lungs serve multiple important life-sustaining functions - making them some of your most important organs. Lung health directly affects every cell in your body!
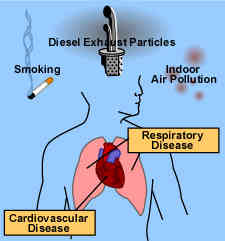
This is why indoor air pollution, smoking, and outdoor air pollution such as smog can have such a far-reaching and damaging affect on your entire body, especially for infants and children, for the elderly, and for those who may already suffer from bad health.
Some of the most common inhallation hazards which can damage your lungs include: pollen, moldspores, bacteria, tobacco smoke, formaldehyde, methylene chloride, hydrogen cyanide, ammonia, particles, hydrocarbons, carbon tetrachloride, benzene, ozone, and bioaerosols.
Unfortunately, the lungs filter out more than just oxygen.
As we've emphasized throughout this website, the air we breath while at home, in the car, at work, or at play is often times not very pure.
Our lungs are frequently exposed to damaging particulates and vapors both man-made and natural. Like home air purifier filters the lungs accumulate particles in direct proportion to the amount of air processed and concentration of pollutants.
Unfortunately, one important difference between your lungs and home air purifiers is that your lungs don't have removable HEPA filters you can simply change when they get dirty!
Particulates and resultant cellular damage tend to accumulate over time so it is important to minimize your exposure to ambient air pollutants through source control, ventillation, and air cleaning.
Fortunately, there are certain built in biological mechanisms involving over three dozen distinct types of lung cells through which the respiratory system attempts to remove particulate contaminants and control cellular damage in the lungs and elsewhere.
One mechanism for removing inhaled particles from the lungs involves cilia which are tiny moving hair like structures that "sweep" the airways clean when possible.
However, tiny sub 0.4 micron particles, which often account for over 90% of inhaled air pollutants, are especially difficult to remove because they travel so deeply into the nooks and crannies of the lungs' alveoli, or air sacs.
These tiniest and most damaging of particles have also been proven to sometimes traverse cell walls and pass into the blood stream via the many small alveolar capillaries. Particles this small are not able to be filter out by most air cleaners, thus control pollutants at their source is very important.
Other particles like Asbestos Fibers can permanantly lodge inside the tiny airways or bronchiols of the lungs causing Asbestosis, Mesothelioma, or Lung Cancer.
The following information about asbestosis and your lungs was provided by the ATSDR, Internet address is www.atsdr.cdc.gov
Top of Page
Asbestos and Your Lungs
Asbestos in Your Attic!? Millions of homes are estimated to be insulated with Zonolite Asbestos-contaminated Vermiculite insulation mined by W.R. Grace & Co. in Libby Montana. Millions of homes are estimated to be insulated with Zonolite Asbestos-contaminated Vermiculite insulation mined by W.R. Grace & Co. in Libby Montana.Is Asbestos Contaminated Vermiculite Insulation Lurking In Your Attic? |
Living With Asbestos-Related Illness
A Self-Care Guide
What is Asbestos?
Asbestos is a rare, naturally occurring mineral with a chainlike crystal structure. Asbestos deposits can be found throughout the world. Deposits are still mined in Australia, Canada, South Africa, and the former Soviet Union. Asbestos is usually found mixed into other minerals. Asbestos is dangerous only if its broken crystal fibers float in the air after being disturbed.
Over the years, asbestos has had many uses. Pipe insulation, automotive brakes, shingles, wallboard, and blown-in insulation are just a few of the products that once contained asbestos. Although the federal government suspended production of most asbestos products in the early 1970s, installation of these products continued through the late 1970s and even into the early 1980s. Asbestos fibers can be released during renovations of older buildings.
 Scanning electron micrograph of asbestos fibers known as asbestiform amphibole fibers |
Nearly everyone is exposed to asbestos at some time in their lives because asbestos fibers have been frequently used in modern industry and they are also found in nature. The fibers float freely. These lightweight fibers can remain in the air for long periods of time.
The risk of developing asbestos-related illness varies with the type of industry in which the exposure occurred and with the extent of exposure.
Generally, asbestos fibers are long, thin, tough, and so small that they cannot be seen. There are two types of asbestos, one is serpentine, which looks like a corkscrew and the other is amphiboles which have long, needle-like fibers. When the fibers float in the air, they are easily inhaled. In most cases the fibers must be breathed in high concentrations over a long period of time to be considered a concern for a person's health.
Asbestos fibers can easily enter the lungs and become trapped in the lung tissues because they are so small. When these fibers are inhaled, they can penetrate and irritate the lungs. White blood cells attack the fiber, and eventually the site becomes scarred. Asbestos fibers break down extremely slowly over time. The fibers can remain in the body for many years and build up in the lungs. Because they attach to the lining of the lungs and airways, the fibers cannot be coughed out or washed out of the lung tissue. The area around the fiber becomes inflamed and, eventually, scarred. As a person's exposure to fibers increases by breathing more fibers, that person's risk of disease also increases. Diseases related to exposure to asbestos do not appear for several years, possibly 15 to 40 years after exposure.
|
Individuals who have been exposed (or suspect they have been exposed) to asbestos dust on the job or at home via a family contact should inform their physician of their exposure history and any symptoms. A thorough physical exam, including a chest x-ray and lung function tests, may be recommended. Interpretation of the chest x-ray may require the help of a specialist who is experienced in reading x-rays for asbestos-related illness. Other tests may be necessary.
Top of PageAsbestos-Related Illnesses
 Microscopic view of mesothelioma cells |
Lung cancer is a malignant tumor that invades and obstructs the lung's air passages. Cigarette smoking greatly increases the likelihood of a person developing lung cancer as the result of asbestos exposure. The most common symptoms of lung cancer are coughing, wheezing and labored breathing. Other symptoms of lung cancer include shortness of breath, persistent chest pain, hoarseness, and anemia as well as weight loss, fever, chills and night sweats. People who develop these symptoms do not necessarily have lung cancer, but they should consult a physician for advice.
Mesothelioma is a very rare cancer of the lining of the chest or abdomen. Most mesotheliomas are caused by exposure to asbestos. By the time they are diagnosed, mesotheliomas are almost always fatal.
Asbestosis is a serious, progressive, long-term disease of the lungs that can get worse as time passes. Asbestosis is not a cancer. It is a disease that restricts how the lungs work, which makes it hard to breathe. Asbestosis is caused by inhaling asbestos fibers that irritate and inflame tissues, which creates scar tissue in the lungs. Along with scarring of the lung tissues, scarring can occur along the lining of the chest wall called the pleura. The scarring makes it hard to breathe and difficult for oxygen and carbon dioxide to pass through the lungs.
 Microscopic view of of lung tissue with asbestosis |
Signs and Symptoms of asbestosis include
- shortness of breath is the primary symptom
- a persistent and productive cough (a cough that expels mucus)
- chest tightness
- chest pain
- loss of appetite
- a dry, crackling sound in the lungs while inhaling.
Asbestosis generally progresses slowly, but the rate of progress can vary greatly from one asbestos exposed person to another. The advancement of symptoms may occur even without additional exposure. It may even speed up with continued exposure. Rapid progression after the first symptoms appear is not common, but it can occur in some people. It can become increasingly difficult to breath as the symptoms progress over time. Lung tissues and the lining of the chest wall can thicken and harden from the thinness and stretchiness of a balloon to that of an orange peel.
As the disease progresses, the individual's shortness of breath becomes more pronounced. The shortness of breath is usually noted first during heavy work or exercise. It will eventually interfere with the ability to carry out everyday activities and the individual may require oxygen. The end result of progression is failure of the lungs and eventual heart failure due to the stress being placed on the heart.
Top of PageThe Respiratory System
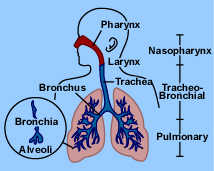
The body needs oxygen to grow and function. The respiratory system is an arrangement of spaces and passageways that bring air into the lungs. These spaces include the nasal cavities; the pharynx, which is used by both the digestive tract and the respiratory system; the voice box or larynx; the trachea or windpipe; and the lungs, which include the bronchial tubes and alveoli (or air sacs).
Nasal Cavities. It is better to breathe through the nose than the mouth because (a) foreign bodies such as dust particles are filtered out by the hairs of the nostrils or caught in the surface mucus, (b) air is warmed by the blood in the vascular membrane, and (c) air is moistened by the mucus in the nasal passage.
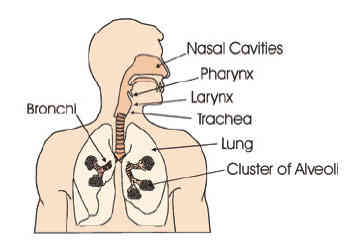 |
Pharynx. The muscular pharynx or throat carries air into the respiratory system tract and also carries foods and liquids into the digestive tract.
Larynx. The larynx, or voice box, is between the pharynx and the trachea. The larynx is lined with little hairs attached to the mucous membranes. The hairs (cilia) trap dust and other particles and move them upward to the pharynx to be expelled by coughing, sneezing, or nose blowing. The cilia are the primary defense of the immune system in the respiratory tract.
Trachea. The trachea, or windpipe, is a tube that extends from the lower edge of the larynx to the upper part of the chest above the heart. The trachea has a framework of cartilage to keep it open. The trachea moves air between the larynx and the lungs.
Bronchi and Bronchioles. The trachea divides into two branches (bronchi), which enter the lungs. The right bronchus is considerably larger than the left and extends downward in a more vertical direction. Each bronchus enters the lung and immediately subdivides again and again, forming smaller divisions. The smallest of the divisions are called the bronchioles.
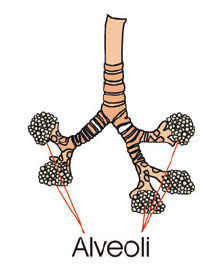 |
Alveoli. At the end of the smallest subdivisions of the bronchioles are clusters of air sacs that look like a bunch of tiny grapes. The sacs are called the alveoli. The average adult lung contains about 600 million alveoli. The exchange of oxygen and carbon dioxide in the blood takes place in the alveoli.
Oxygen-rich blood is sent to the heart, which pumps it through the body. The red blood cells carry carbon dioxide to the alveoli, and then the carbon dioxide leaves the body through exhaled breath.
Breathing that is too shallow, slow, or the result of reduced lung function is called hypoventilation. Hypoventilation results in inadequate oxygenation of the blood. Respiratory obstruction, lung disease, or exposure to toxicants can also cause this condition.
Top of PageAmazing Facts About the Lungs
- The right lung is slightly larger than the left.
- Hairs in the nose help clean and warm the air we breathe.
- The surface area of the lungs is roughly the same size as a tennis court.
- The capillaries in the lungs would extend 994 miles (1,600 kilometers) if placed end to end.
- The highest record "sneeze speed" is 102.5 miles (165 kilometers) per hour.
Asbestos fibers enter the body from the air we breathe. Most of the small particles we breathe— like dust and pollen—are stopped or trapped by the mucous lining and nasal hairs before entering the small airways of the lungs . Because asbestos fibers are so small and thin, they pass all the way down to the small airways and alveoli (or air sacs), where the oxygen-carbon dioxide gas exchange occurs.
The immune system, the body's defense system, considers asbestos fibers foreign invaders and tries to break them down and remove them from the lung.
Top of PageBreakdown Process
Each alveolus has many cleaning cells, called macrophages, that destroy foreign invaders in the alveoli. Because asbestos fibers are too long and sharp, macrophages cannot destroy them. Macrophages then try to surround the fiber so that it cannot cause damage. In doing so, the macrophage is essentially cut open and its digestive molecules are spilled on the alveoli. This causes scar tissue to form in the spaces around the small airways and alveoli.
Scarring and thickening of the lung tissue decreases the ability of the lungs to exchange oxygen and carbon dioxide between the alveoli and the blood cells, so breathing becomes more difficult.
Top of PageTreatment of Asbestos Related Illness
Unfortunately, no cure exists for asbestosis. Treatment involves preventing further complications of the disease and treating its symptoms. For information about cancer treatment, contact the National Cancer Institute's Cancer Information Service, whose toll free number is 1-800-4-CANCER.
Top of PageRespiratory Infections
People with chronic lung diseases such as asbestosis are more susceptible to respiratory infections because the lungs are already damaged. One of the most important preventative measures is to produce a productive cough, or a cough that brings up mucus.
It is important to cough effectively to clear out the air passages. An effective cough is moist and brings mucus up from the lungs and air passageways. An ineffective cough reduces airflow and causes respiratory muscle fatigue. If mucus and other foreign bodies remain in the respiratory tract, they can pool in the airways, making it difficult to expel bacteria and increasing the risk of infection.
Your doctor will probably recommend a humidifier, breathing therapies, and chest percussion to ensure a productive cough. Very dry air increases shortness of breath and thickens the mucus in your lungs. These steps loosen and thin out bronchial secretions, allowing them to be expelled by the cough.
Make an effort to prevent infection. People with asbestosis should receive aggressive medical care, including frequent use of antibiotics when warranted, for any respiratory infection.
Top of PageTake Care of Yourself To Prevent Infection
Keep a diary of when you have trouble breathing. Note how often you have trouble, how bad it is, and what you were doing before you had trouble. The diary will help you recognize and avoid events that trigger breathing trouble.
Stay inside, if possible, when air pollution and pollen counts are high. An air-filtering machine can improve the indoor air quality in your home.
Avoid breathing pollutants that can aggravate shortness of breath. Such pollutants include fumes from heavy traffic, smog, aerosol sprays, and products that produce chemical vapors (for example, paint, kerosene, and cleaning agents).
In cold weather, breathe through your nose and cover your mouth and nose with a scarf.
Exercise is important to increase the strength and endurance of the respiratory muscles. Increased physical activity increases respiratory muscle strength.
Drink lots of fluids—at least six glasses of water daily, unless your doctor tells you differently.
Eat healthy foods including lots of fruits and vegetables. Poor eating habits result in smaller muscle mass and are an enemy of the patient with respiratory disease.
Take measures to correct an anemic condition and/or electrolyte imbalance in your blood. Such measures could improve cardiopulmonary performance.
Watch your salt intake. Keep it low.
Breathe slowly.
To lower your risk of colds or flu, wash your hands often.
Get flu and pneumonia vaccinations every year (between September and December). Caregivers and all household members, whether or not they provide care, also should be vaccinated.
Avoid situations that might expose you to respiratory infections (for example, large crowds).
Follow your doctor's instructions on taking your medicines, oxygen therapy, and/or chest physiotherapy.
Sleep 7 or 8 hours every night.
Take several short rests during the day. Learn to conserve your energy and avoid getting too tired.
Take special precautions with your personal hygiene. Wash your hands before taking your medication or handling your oxygen equipment.
Do not try to treat yourself. Over-the-counter cold remedies might worsen the problem, so do not use them unless your doctor tells you it is okay.
Have regular chest x-rays to screen for cancers associated with asbestos exposure.
Call your doctor if any of the following signs occur:
- Fever
- Increased coughing, wheezing, or breathing
- Changes in mucus (mucus is thicker; either more or less mucus is present than usual; mucus has a foul odor; or mucus is green, yellow, brown, pink, or red)
- Stuffy nose, sneezing, or sore throat
- Increased fatigue or weakness
- Weight gain or loss of more than 6 pounds within a week
- Swollen ankles or feet.
Symptoms of respiratory infections can appear suddenly and worsen quickly. When an infection develops, it is important to start treatment right away. Your doctor might prescribe antibiotics or other drugs to get the infection under control before it becomes serious. See your doctor as soon as you feel sick.
Top of PageSelf-Care
No cure exists for asbestosis, but taking care of yourself can help you maintain a more comfortable life. Some self-care tips and techniques follow.
- Stay away from smoke and smokers. If you smoke, now would be a good time to quit. Smoking can increase the rate of disease progression, and it also increases the risk of lung cancer. Even if you have been smoking for years—or you already have lung disease— quitting smoking now will greatly improve your health. The tracheal cilia will begin working again and help keep your lungs swept clean. The blood vessels will relax, allowing the blood to flow normally, so your heart will no longer have to work as hard. The lung tissue will become healthier and you will breathe easier.
A structured program has a good chance of successfully helping smokers quit the habit. Recent trials using the nicotine patch and antidepressants have been shown to be more effective than counseling in helping smokers quit. - Participate in respiratory therapies (such as bronchial drainage) as recommended by your doctor. Your doctor might recommend using an ultrasonic mist humidifier that assists in clearing secretions from the lungs. Respiratory treatments that remove secretions from the lung through postural drainage might also be used.
- Proper training and adherence to decontamination techniques can minimize the risk of infection associated with respiratory therapy devices.
- Clean all reusable respiratory therapy equipment such as ventilator circuitry, nebulizers, aerosol tubing, and peak flow meters twice weekly. Consult your provider about cleansing routines for respiratory equipment.
- All cleaned devices must be allowed to air dry thoroughly before reassembling for use. Moisture trapped in the devices can be a potential reservoir for bacteria, viruses and fungi
- All ventilator filters should be cleaned and changed as often as the manufacturer recommends.
Oxygen. If your doctor has prescribed oxygen, you will have a liquid oxygen unit, an oxygen tank, or an oxygen concentrator. You will breathe the oxygen through either a mask or nasal cannulae (two short prongs that fit just inside your nostrils). The system will also have a humidifier to warm and moisten the oxygen.
It is a good idea to also have a small portable oxygen tank available in case of power failure.
Only your doctor can determine how much oxygen you need. You should never change the flow rate without instructions from your doctor. The medical supply company will show you how to set the flow rate and how to care for the equipment. Keep the supplier's telephone number handy so you can call if the system does not work properly.
Sometimes it is hard to tell whether oxygen is flowing through the tubes. If you have doubts, check to be sure that the system is turned on and the tubing does not have any kinks. If you still are not sure, place the nasal cannulae in a glass of water with the prongs up and watch for bubbles. If no bubbles appear, oxygen is not flowing through the tubes and you need to call your supplier.
Oxygen is very combustible. Be sure to keep your oxygen unit away from open flames and heat, including lit cigarettes, gas stoves, space heaters, or kerosene heaters.
When traveling around town, be sure to plan for an adequate supply of oxygen and know how much time you can safely travel between refills. Always allow for a 20%–25% safety margin to cover any unexpected delays. When traveling, keep the oxygen container upright and secure at all times.
Traveling With Oxygen
- Discuss your travel plans with your doctor to be sure it is all right for you to travel and to find out how long your trip can be.
- Contact your oxygen supply company about your travel plans. The company will recommend the equipment you need and help determine the time you can safely travel between refills. Get the oxygen equipment with which you will travel ahead of time so you can become familiar with how to operate it. Your supplier can also arrange to have oxygen supplied to you at your destination.
- Check with your insurance company. You may have to pay in advance for equipment and submit the insurance claims after you return home. Be sure to keep your receipts.
- Always keep your prescription with you throughout the trip.
Traveling by Bus
Bus lines do permit travel with oxygen equipment. However, to prevent any unexpected problems, check in advance. Most bus companies permit you to take one E cylinder onto the bus, but extra tanks are not allowed in the baggage compartment. You must be able to put your tank on and take it off by yourself.
Traveling by Train
Make reservations with Amtrak at least 4 days in advance, even for short trips. You may bring two cylinders, either size E or F, and the oxygen unit must be self-contained and not on wheels. On overnight trips, you must have a sleeper compartment, where you are required to stay while using oxygen. Meals can be sent to your sleeper.
Traveling by Ship
Cruise line regulations differ and are subject to change, so you must contact the cruise line regarding current rules. Some cruise lines permit you to travel only with oxygen cylinders and limit the number you may bring on board. Be prepared to supply the following information from your doctor: a prescription stating the quantity of oxygen and the flow rate, a letter describing your diagnosis, and a statement that you are approved for travel.
Traveling by Plane
Regulations vary from one airline to another and are subject to change. Always call ahead of time to inquire about current rules. Some airlines will not permit passengers to use oxygen. Others airlines are willing to provide oxygen if you make advance arrangements, but you must use their oxygen supply. Airlines do not allow passengers to bring oxygen on board the plane. Always bring your own nasal prongs: some airlines use only simple oxygen masks, which allow carbon dioxide buildup. Also bring a nipple adapter that fits all tubing.
You must make reservations 2 to 5 days in advance, depending on the individual airline's rules. Be sure to ask what documents you will need to supply. Airline documentation requirements are similar to those of cruise lines, and some airlines also have special forms that must be filled out by your doctor. You might have to sign a liability statement. In a few cases, you are required to bring a companion with you on the flight. Additional charges vary, but expect to pay about $50 extra.
Allow at least 1 hour between connecting flights. Remember that you must arrange for oxygen for the time between flights. Local oxygen suppliers will provide this service for layovers between flights. Whenever possible, use small airports because they usually have fewer delays and their boarding gates are closer together.
Lodging
Hotels and motels are usually very accommodating about special needs. Someone is usually available to transport your oxygen tank. Contact your local supply company about arranging for a supply company at your destination to set up the equipment in the room before you arrive.
Relaxation and Breathing Techniques
The feeling of not being able to get enough air into your lungs is frightening. Breathing training is aimed at controlling the respiratory rate and breathing pattern, thus decreasing the risk that used air will not stay in your lungs. Breathing training also attempts to improve the position and function of the respiratory muscles and effectiveness of coughs.
You can do exercises to help you breathe more easily. Practice the exercises daily so that when you are having problems with shortness of breath, you will do them naturally and not panic.
- Pursed-Lip Breathing: Pursed-lip breathing will slow down your breathing so that it is more efficient (breathing fast only worsens shortness of breath). Pursed-lip breathing can be done anywhere.
- Breathe in slowly through your nose. Hold your breath for 3 seconds.
- Purse your lips as if you are going to whistle.
- Breathe out slowly through your pursed lips for 6 seconds.
- Abdominal/Diaphragm Breathing: Abdominal breathing also slows down your breathing and helps relax your entire body.
- Lie on your back in a comfortable position with a pillow under your head and knees.
- Rest one hand on your abdomen just below your rib cage. Rest the other hand your chest.
- Slowly breathe in and out through your nose using your abdominal muscles. The hand resting on your abdomen will rise when you breathe in and fall when you breathe out. The hand on your chest should be almost still. Repeat three or four times before resting.
- Active Cycle of Breathing Technique (ACBT): ACBT should be discussed with your doctor before implementation. ACBT is a series of breathing techniques that help clear secretions and improve aeration (the delivery of air to the alveoli [air sacs]). ACBT can be done sitting upright. This technique combines breathing exercises with the huff cough and has three components in a set cycle. The cycle is repeated until the huff becomes dry or nonproductive, or when 20 minutes have passed. Ask your doctor for instructions on this therapy
Pulmonary Rehabilitation
Patients with advanced lung disease may have emotional disorders, mainly depression and anxiety. In addition to appropriate medical therapy for theses disorders, exercise such as a pulmonary rehabilitation program can help lessen these feelings.
Talk to your doctor about participating in a pulmonary rehabilitation program. Pulmonary rehabilitation uses different therapeutic components for persons with pulmonary disease. The goal of pulmonary rehabilitation is achieving and maintaining the patient's maximum level of independence and functional ability in the community.
Pulmonary rehabilitation is becoming a crucial component of the overall therapy of many patients. It offers the best treatment option for patients with chronic respiratory illnesses. Pulmonary rehabilitation has helped people achieve increased exercise capacity and endurance; improved health-related quality of life; decreased shortness of breath; and fewer hospital admissions, even among patients with the most severe degree of lung disease.
The goals of a pulmonary rehabilitation program are to
- Reduce work of breathing
- Improve pulmonary function
- Alleviate shortness of breath
- Increase efficiency of energy use
- Correct nutrition deficiencies
- Improve exercise performance and daily activities
- Restore a positive outlook
- Improve emotional state
- Decrease health-related costs
- Improve survival.
If you are interested in pulmonary rehabilitation, ask your doctor to help you design a program that will work for you.
References
Agency for Toxic Substances and Disease Registry. (2000); Asbestos and your health [fact sheet]. Atlanta: US Department of Health and Human Services.
American Lung Association. 2000. Asbestosis. New York: American Lung Association. Available from URL: www.cheshire-med.com/programs/pulrehab/asbestosis.html
Bartholomew D, Gainey A, Louie W, Phillips C, Sonnek N. 1999. Asbestosis. Omaha (NE): Creighton University School of Medicine. Available from URL: www.medicine.creighton.edu/forpatients/Asbestosis/Asbestosis.html
Children's Hospital of Eastern Ontario. 1999. Assisted airway clearance for Immotile Cilia syndrome. Ottawa, Ontario, Canada: Children's Hospital of Eastern Ontario. Available from URL: www.cheo.on.ca./pcdc/pcdc_physio.htm.
Cohen BJ, Wood DL, Memmler RL. 2000. Memmler's the human body in health and disease. Philadelphia: Lippincott, Williams & Wilkins.
Cohen BJ, Wood DL. 2000. Memmler's the structure and function of the human body. Philadelphia: Lippincott, Williams & Wilkins.
Galvin JR, D'Alessandro MP. 1994. Electric Diffuse Lung: the diagnosis of diffuse lung disease. Asbestosis. Iowa City (IA): University of Iowa College of Medicine Virtual Hospital. Available from URL: www.vh.org/Providers/Textbooks/DiffuseLung/Text/Asbestosis.html.
Lewis SR, Heitkemper MM, Dirksen SM. 2000. Medical/surgical nursing: assessment and management of clinical problems. 5th edition. St. Louis (MO): Mosby-Year Book.
Harrison A, editor. 1995. Mosby's patient teaching guide. St. Louis (MO): Mosby-Year Book. National Cancer Institute. 1996. Questions and answers about asbestos exposure: CancerNet from the National Cancer Institute. Bethesda (MD): National Cancer Institute. Available from URL: www.graylab.ac.uk/cancernet/600321.html.
Springhouse Corporation. 1998. Anatomy and physiology: a health care professional guide. Springhouse (PA): Springhouse Corporation.
Springhouse Corporation. 1998. Diseases: a health care professional guide. Springhouse (PA): Springhouse Corporation.
Top of PageThis guide provides the patient living with asbestos-related illnesses and his or her family with skills and information to help them adapt and cope with their illness. For more information, contact ATSDR's toll-free information line: (888) 42-ATSDR. . . that's (888) 422-8737. The information in this guide is courtesy of:
ATSDR - Internet address is www.atsdr.cdc.gov
The needle-like structure of asbestos makes it a particularly pernicious inhalation hazard because it "stabs" the tissues, which fixes asbestos crystals inside the lungs permantly. This often leads to the buildup of scar tissue which interfers with gaseous exchange and makes it harder to breath.
Smokers who have been exposed to asbestos are also far more likely to develop lung cancer or bronchial carcinoma.
Of course for smokers of Kent cigarettes in the early 1950's both asbestos and cigarette smoke were delivered simultaneously to some smokers' lungs since the cigarettes were manufactured using "filters" that contained asbestos fibers!
Radon is also a major cause of lung cancer second only to smoking. As with asbestos exposure, radon exposure increases lung cancer risk emmensely.
The decay products of radon gas are radioactive toxic charged particles which become attached to indoor second-hand smoke particles and thus can be inhaled deeply into the lungs where their radiation causes the most damage to lung tissue cells.
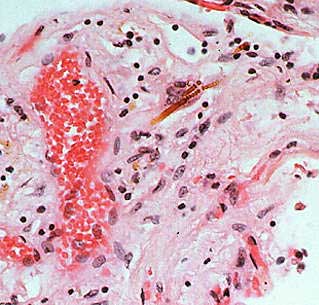

To the above left is a picture of lung tissue containing asbestos crystals which are often the cause of Asbestosis, mesothelioma, or asbestos lung cancer. To the above right is a picture of lung with Emphysema (also known as COPD or Chronic Obstructive Pulmonary Disorder). The picture of smoker lung illustrates how cigarette smoke damages your lungs. The single most important action someone could do to improve all aspects of not only the health of their lungs but their entire body is to:
Top of Page
Learn More About Asbestos and Your Lungs:
Is deadly Asbestos lurking in your home? Also don't miss our Asbestos section of our HUGE Household Chemical Guide which includes information on over 100 other potentially hazardous household chemicals - It's one of the largest guides to household chemical hazards available on the internet! |
Top of Page
As discussed above, eventually asbestos exposure may lead to deadly Mesothelioma whereby cells become cancerous in the protective membrane which lines most of the internal organs. This membrane is known as the Mesothelium.
The membrane lining the chest cavity and lungs, known as the Pleura, is the most likely site where Mesothelioma occurs.
However, the lining of the abdominal cavity, the Peritoneum, and the membrane protecting the heart, the Pericardium, are also target sites for Mesothelioma to develop.
Estimates suggest that the number of cases of Mesothelioma in 2004 were about 15 per million people in the United States and as much as 40 Mesothelioma cases per million people in other Industrialized nations. Unfortunately cases in developing nations continues to increase.
Another mechanism for removing inhaled irritants such as cigarette smoke, dust, pollen, noxious fumes, or water is via coughing or sneezing.
The airways of the respiratory system contain special nerves which can detect the presence of these inhaled irritants. These nerves then send signals to the respiratory centers causing a rapid contraction of the muscles surrounding the lungs which causes the air in the lungs to be violently exhaled at speeds as high as 100 mph to "flush" out the particles. When these same respiratory centers overstimulated the diaphram we experience hiccups.
Because of the very high amount of surface area for gas exchange in the lungs' alveolar air sacs, the lungs are the point at which the outside air most efficiently contacts our internal tissues.
It is no wonder there is such a wide variety of lung diseases and conditions which can results from inhaling damaging vapors or particles.
Trauma to the lungs and congenital lung defects can also result in specific lung conditions. No matter the source, most lung ailments interfer with either the lungs' ability to exchange oxygen for carbon dioxide or the lungs' ability to function mechanically thus making it harder to breath.
Apnea, Asthma, Bronchitis, Emphysema, and Pneumothorax are conditions that interfer with the lungs' mechanics of breathing.
Carbon Monoxide Poisoning, Pulmonary Adema, and Smoke Inhalation are conditions which usually interfer with the lungs ability to exchange gases.
Top of Page
Other Forms of Lung Disease:
Learn which toxic chemicals are likely to cause many of these Respiratory and Lung DiseasesAcute Respiratory Distress Syndrome (ARDS) |
Top of Page
Effects of Air Pollutants on Your Lungs
- Exposure to air pollution is associated with numerous effects on human health, including pulmonary, cardiac, vascular, and neurological impairments.
- The health effects vary greatly from person to person.
- High-risk groups such as the elderly, infants, pregnant women, and sufferers from chronic heart and lung diseases are more susceptible to air pollution.
- Children are at greater risk because they are generally more active outdoors and their lungs are still developing.
- Exposure to air pollution can cause both acute (short-term) and chronic (long-term) health effects.
- Acute effects are usually immediate and often reversible when exposure to the pollutant ends.
- Some acute health effects include eye irritation, headaches, and nausea.
- Chronic effects are usually not immediate and tend not to be reversible when exposure to the pollutant ends.
- Some chronic health effects include decreased lung capacity and lung cancer resulting from long-term exposure to toxic air pollutants.
- The scientific techniques for assessing health impacts of air pollution include air pollutant monitoring, exposure assessment, dosimetry, toxicology, and epidemiology.
- Although in humans pollutants can affect the skin, eyes and other body systems, they affect primarily the respiratory system.
- Air is breathed in through the nose, which acts as the primary filtering system of the body.
- The small hairs and the warm, humid conditions in the nose effectively remove the larger pollutant particles.
- The air then passes through the pharynx, esophagus, and larynx before reaching the top of the trachea.
- The trachea divides into two parts, the left and the right bronchi.
- Each bronchi subdivides into increasingly smaller compartments.
- The smallest compartments of the bronchi are called bronchioles, which contain millions of air sacs called alveoli.
- Together, the bronchioles and alveoli make up the lungs.
- Both gaseous and particulate air pollutants can have negative effects on the lungs.
- Solid particles can settle on the walls of the trachea, bronchi, and bronchioles.
- Most of these particles are removed from the lungs through the cleansing (sweeping) action of "cilia", small hairlike outgrowths of cells, located on the walls of the lungs. This is what occurs when you cough or sneeze.
- A cough or sneeze transports the particles to the mouth.
- The particles are removed subsequently from the body when they are swallowed or expelled.
- However, extremely small particles may reach the alveoli, where it takes weeks, months, or even years for the body to remove the particles.
- Gaseous air pollutants may also affect the function of the lungs by slowing the action of the cilia.
- Continuous breathing of polluted air can slow the normal cleansing action of the lungs and result in more particles reaching the lower portions of the lung.
- The lungs are the organs responsible for absorbing oxygen from the air and removing carbon dioxide from the blood-stream.
- Damage to the lungs from air pollution can inhibit this process and contribute to the occurrence of respiratory diseases such as bronchitis, emphysema, and cancer.
- This can also put an additional burden on the heart and circulatory system.
- Hazardous air pollutants may cause other less common but potentially hazardous health effects, including cancer and damage to the immune system, and neurological, reproductive and developmental problems.
- Acute exposure to some hazardous air pollutants can cause immediate death.
- Human health effects associated with indoor air pollution are: headaches, tiredness, dizziness, nausea, and throat irritation.
- More serious effects include cancer and exacerbation of chronic respiratory diseases, such as asthma.
- Radon is estimated to be the second leading cause of lung cancer in the U.S.
- Environmental tobacco smoke causes eye, nose and throat irritation, and is a carcinogen.
- Asthma, particularly in children, is associated with poor indoor air quality.
Top of Page
Air Pollutants Toxic to Your Lungs
The following is a summary of some of the most common forms of air pollutants which may damage your lungs and which you may be exposed to at home, work, or play. Most of these pollutants are referred to as Criteria pollutants by the EPA because their sources are commonly widespread all over the United States.
Dust / Particulate Matter (PM) and Your Lungs
- PM can be a primary or secondary pollutant consisting of very small particles of soot, dust, or other matter, including tiny droplets of liquids.
- "Primary" particles of PM, such as dust or black carbon (soot) are directly emitted into the air and come from a variety of sources such as cars, trucks with diesel engines, buses, power plants, factories, construction sites, tilled fields, unpaved roads, stone crushing, and burning of wood.
- "Secondary" particles of PM are formed in the air from the chemical change of primary gaseous emissions and are formed indirectly when gases from burning fuels react with sunlight and water vapor.
- Secondary PM can result from fuel combustion in motor vehicles, at power plants, and in other industrial processes.
- PM2.5 describes the "fine" particles that are less than or equal to 2.5 µm in diameter.
- PM10 refers to all particles less than or equal to 10 µm in diameter (about one-seventh the diameter of a human hair).
- Health Effects of Particulate Matter or dust inhalation include: eye irritation, asthma, bronchitis, lung damage, cancer, heavy metal poisoning, cardiovascular effects.
- Particulate Matter such as dust and soot also cause: visibility impairment, atmospheric deposition, aesthetic damage.
- Respirable dust particles and other particulates like Bioaerosols are some of the most common indoor air pollutants in your home and workplace.
- When fine dust enters the respiratory system, the human body considers it to be foreign material which should be defended against.
- The main effects of dust on health are an inflammatory response (chronic irritation) or a toxic response.
- In effect the particles of dust act as a poison to the cells they come in contact with.
- Rarely does it cause an altered immune response of the system.
- The purpose of the respiratory system is to allow air to come into intimate contact with the blood system in order to exchange oxygen and carbon dioxide.
- The lungs are well protected against dust by many filters located in the nose and respiratory channels which trap particles before they reach the bronchi and lung alveoli.
- Three main factors need to be considered when assessing the risks associated with dust:
- (1) penetration
- (2) reaction
- (3) health effects
- The aerosol particles have to penetrate the respiratory system.
- The particles must be small enough and the particle concentration has to be high enough to defeat the defence mechanisms, or the dust must be toxic.
- When the particles penetrate the respiratory system, there will be a reaction to the intruding particles.
- Basically, there are two types of reaction: the immediate symptoms, and the delayed symptoms.
- The immediate symptoms of a respiratory allergy can be eye irritation, nasal stuffiness, a streaming nose or an itchy throat.
- The delayed symptoms include headache, dizziness, nausea, breathlessness, fever, and vomiting, leading to unproductive coughing and breathing difficulties.
- These symptoms usually appear 3 to 4 hours after exposure, reach a peak in 7 to 8 hours and disappear after 24 hours.
- "Farmer's Lung" and "Organic Dust Toxic Syndrome" are examples of delayed hypersensitivity of the respiratory system to specific dust.
- There are three categories of health effects.
- First, there can be some temporary damage to the respiratory system which will disappear rapidly when the person is no longer exposed to dust.
- Second, there can be the occurrence of insidious damage to the respiratory system such as bronchitis or occupational asthma after long-term exposure to dust.
- The reaction is not as explosive as an allergic reaction, but has various symptoms such as coughing, shortness of breath, or a reduction of pulmonary capacity.
- However, when a person is no longer exposed, the respiratory system may, but not always, recover entirely.
- Third, permanent lung damage can occur without showing any allergic reactions when you are continuously exposed to dust for long periods of time.
- This means that some parts of their lung tissue are permanently affected reducing respiration capacity; unfortunately, this process is irreversible.
Top of Page
 |
Top of Page
What Happens When Dust is Inhaled into the Lungs?
1. Dust particles are inhaled through the nose or throat.
2. Millions of these dust particles strike and stick to the moist surfaces of:
- a. Nasal passage (particles that are 10 microns and larger)
- b. Trachea (particles that are 5 to 10 microns)
- c. Bronchi (particles that are 5 to 10 microns)
- d. The smallest cavities of the lung - the alveoli (particles that are less than 5 microns)
3. In all these organs, repeated or heavy exposure to organic dusts may induce an allergy to substances in these dusts. And any further contact, even with small amounts, can then produce such symptoms as asthma, fever, general tiredness and shortness of breath.
4. The worst damage can be done by the smaller of the fine particles which reach the finest lung space - the alveoli. Unfortunately, studies have repeatedly proven that over 90% of indoor air pollutants such as dusts, viruses, bacteria, vapors, and other aerosols are of this size (less than 0.3 microns). Worse yet these smallest and most common of particles also tend to be the most toxic to the lungs and body due to not only their contact with the alveoli, but also due to their typical toxic composition.
The best air purifier for these finest and most damaging of dust and aerosol particles must have efficient HEPA and Gas-phase filtration in order to be truely effective for cleaning air.
Top of Page
Nitrogen Oxides (NOx) / Nitrogen Dioxide (NO2) and Your Lungs
 |
- Nitrogen Oxides (NOx), is the generic term used to describe the sum of NO, NO2 and other oxides of nitrogen.
- NOx is a group of highly reactive gases that play a major role in the formation of ozone.
- Many of the nitrogen oxides are colorless and odorless; however, one common pollutant, nitrogen dioxide (NO2) along with particles in the air can often be seen as a reddish-brown layer over many urban areas.
- Nitrogen oxides form when fuel is burned at high temperatures, as in a combustion process.
- The primary sources of NOx are motor vehicles, electric utilities, and other industrial, commercial, and residential sources that burn fuels.
- Nitrogen Dioxide is a reddish brown, highly reactive gas.
- Sources of Nitrogen Dioxide include: Motor vehicles, electric utilities, and other industrial, commercial, and residential sources that burn fuels.
- Some health effects of Nitrogen Dioxide inhallation include: Susceptibility to respiratory infections, irritation of the lung and respiratory symptoms (e.g., cough, chest pain, difficulty breathing).
- Nitrogen Dioxide may also contribute to the formation of smog, acid rain, water quality deterioration, global warming, and visibility impairment.
Top of Page
Carbon Monoxide (CO) and Your Lungs
- Carbon Monoxide (CO), is a colorless, odorless gas formed when carbon in fuel is not burned completely.
- Motor vehicle exhaust contributes about 60 percent of all CO emissions nationwide (Latest Finding on National Air Quality 2002).
- Other non-road engines and vehicles (such as construction equipment and boats) contribute about 22 percent of all CO emissions nationwide.
- Higher levels of CO generally occur in areas with heavy traffic congestion.
- In cities, 95 percent of all CO emissions may come from motor vehicle exhaust.
- Other sources of CO emissions include industrial processes (such as metals processing and chemical manufacturing), residential wood burning, and natural sources such as forest fires.
- Some common sources of Carbon Monoxide indoors are: motor vehicle exhaust, kerosene or wood burning stoves, gas stoves, cigarette smoke, and space heaters
- The highest levels of CO in the outside air typically occur during the colder months of the year when CO automotive emissions are greater and nighttime inversion conditions are more frequent.
- In inversion conditions the air pollution becomes trapped near the ground beneath a layer of warm air.
- Some health effects of Carbon Monoxide inhallation include: headaches, reduced mentalalertness, heart attack, cardiovascular diseases, impaired fetal development, or death.
- Carbon Monoxide is a common contributor to the formation of smog.
Top of Page
Ozone (O3) and Your Lungs
- Ozone (O3) is a gas composed of three oxygen atoms and it is also a colorless compound that has an electric-discharge-type odor.
- Ozone is a unique criteria pollutant in that it is exclusively a secondary pollutant not usually emitted directly into the air.
- Ozone is created at ground level by a chemical reaction between oxides of nitrogen (NOx) and volatile organic compounds (VOCs) in the presence of heat and sunlight.
- The concentration of ozone in a given locality is influenced by many factors, including the concentration of NO2 and VOCs in the area, the intensity of the sunlight, and the local weather conditions.
- Ozone and the chemicals that react to form it can be carried hundreds of miles from their origins, causing air pollution over wide regions.
- Ozone has the same chemical structure whether it occurs miles above the earth or at ground level and can be "good" or "bad," depending on its location in the atmosphere.
- "Good" ozone occurs naturally in the stratosphere and forms a layer that protects life on earth from the sun's harmful rays or ultraviolet radiation.
- In the earth's lower atmosphere, or troposphere, ground-level ozone is considered "bad".
- Ozone is the most prevalent chemical found in photochemical air pollution, or smog.
- Sources of Ozone are vehicle exhaust and certain other fumes.
- Ozone may also be formed from other air pollutants in the presence of sunlight.
- Some home air purifiers known as Ozone Air Cleaners emit Ozone gas intentionally. Ozone purifiers may also be marketed using the term "activated oxygen" in place of ozone, but they are still ozone emitters just the same.
GOVERNMENT AGENCIES SUCH AS THE EPA SAY THESE OZONE HOME AIR PURIFIERS ARE TO BE AVOIDED BY HOMEOWNERS! - Learn about the new breakthrough technology in ionic air purifiers that is Ozone free yet very effective. Leave it to those tech savvy Japanese at the Sharp Corporation to finally bring us the best ionizing air cleaner that actually work, unlike those other dangerous and ne'er do well ionizers known as Ozone Air Purifiers. Visit our introduction to this advanced home appliance: Sharp Plasmacluster FPN60CX Air Purifier - Ozone Free, Quiet, and Powerful ionizing air cleaner.
- Some health effects of Ozone inhallation include: eye and throat irritation, coughing, respiratory tract problems, asthma, lung damage, and Asthma.
- Ozone is especially known to make asthma worse, make the lungs work less effectively, inhibit the development of childrens' lungs, and thus Ozone may also contribute to the onset of Asthma in children.
- Ozone gas may also cause plant and ecosystem damage.
- Ozone is made of three oxygen atoms (O3), while the air contains oxygen that is made up of only two atoms (O2).
- Ozone is inherently unstable; therefore, ozone wants to break down and return to the more stable O2 form.
- Ozone's instability as a molecule is what may lead to some of the ill effects that ozone can have on our health.
Sulfur Dioxide (SO2) and Your Lungs
- Sulfur Oxides (SOx) are colorless gases formed by burning sulfur.
- SOx gases are formed when fuel containing sulfur, such as coal and oil, is burned, and when gasoline is extracted from oil or metals are extracted from ore.
- Sulfur dioxide (SO2) is the criteria pollutant that is the indicator of sulfur oxide concentrations in the ambient air.
- SO2 dissolves in water vapor to form acid, and interacts with other gases and particles in the air to form sulfates and other products that can be harmful to people and their environment.
- Over 65% of SO2 released to the air, or more than 13 million tons per year, comes from electric utilities, especially those that burn coal.
- Other sources of SO2 are industrial facilities that derive their products from raw materials like metallic ore, coal, and crude oil, or that burn coal or oil to produce process heat. Mercury is another toxic byproduct of the coal burning industry. For much more specific information about Mercury visit our Mercury Bible.
- Some specific examples of Sulfur Dioxide producers are: manufacturers of sulfuric acid, smelters of ores containing sulfur, petroleum refineries, cement manufacturing, metal processing facilities, locomotives, large ships, and some nonroad diesel equipment burning high sulfur fuels.
- Some health effects caused by Sulfur Dioxide inhallation include: eye irritation, wheezing, chest tightness, shortness of breath, and lung damage.
- Sulfur Dioxide gas may also contribute to the formation of acid rain, visibility impairment, plant and water damage, and aesthetic damage.
- One air pollution disaster involving Sulfur Dioxide in 1930 Meuse River Valley, Belgium resulted in the death of 63 people and thousands sick when a temperature inversion increased Sulfur Dioxide levels in the atmosphere.
Top of Page
Lead (Pb) and Your Lungs
- Lead is a biologically toxic metallic element now found in everyone's blood.
- Since the phase-out of Lead addition to gasoline the common sources of Lead have become: metal refineries, lead smelters, lead-acid battery manufacturers, and iron and steel producers.
- Some common health effects of Lead exposure include: anemia, high blood pressure, brain and kidney damage, neurological disorders, cancer, and lowered IQ.
- Lead is also an environmental hazard which affects animals, plants, and aquatic ecosystems.
- Our Lead Bible is a wealth of public health information about Lead sources, Lead diseases, Lead toxicology, Lead MSDS, and Lead FAQs.
Top of Page
Endotoxins and Your Lungs
Endotoxins are compounds that are on some common bacteria (in the outer membrane) and can trigger an allergic response.Endotoxin exposure has been shown to be related to adult asthma, so it may also play an important role in childhood asthma.The NIEHS currently is examining how childhood exposure to endotoxins relates to developing asthma and other respiratory diseases.
There are hundreds of potential sources of Endotoxins in the average home. Visit our extensive chart of bioaerosols to learn about specific sources of these Endotoxins lurking in your indoor air.
The Agricultural Health Survey is assessing various exposures, including endotoxin exposure, in children and how they relate to developing respiratory disorders and several other diseases. Additionally, one of the Children's Health Centers is evaluating the role of infection by Respiratory Syncytial Virus (a common viral infection during the first year of life) in the response of airways of the lungs to endotoxins. Together, these studies should give us a better idea about how the amount, time, and length of exposure to endotoxins can affect the development of respiratory diseases.
Acronyms Related to Lungs and Your Health:
- ADHD Attention Deficit/Hyperactivity Disorder
- NIDDK National Institute of Diabetes and Digestive and Kidney Diseases
- CDC Centers for Disease Control and Prevention
- NIEHS National Institute of Environmental Health Sciences
- DEHP Di(2-ethylhexyl) phthalate
- NIH National Institutes of Health
- EPA United States Environmental Protection Agency
- NIMH National Institute of Mental Health
- FDA Food and Drug Administration
- NINDS National Institute of Neurological Disorders and Stroke
- HUD Department of Housing and Urban Development
- NINR National Institute of Nursing Research
- NCI National Cancer Institute
- NTP National Toxicology Program
- NIA National Institute of Aging
- OBSSR Office of Behavioral and Social Sciences Research
- NIAID National Institute of Allergy and Infectious Diseases
- PA Program announcement
- NICHD National Institute of Child Health and Human Development
- PCB Polychlorinated biphenyls
- NIDCD National Institute of Deafness and Communication Disorders
- RFA Request for applications
Top of Page
Organizations For More Information About Your Lungs:
I hope you found the following information about your lungs and lung diseases helpful. Please Contact the Home Air Purifier Expert if you have any comments or questions about lungs, the Respiratory System, or Lung Health.
Return to Home Air Purifier Index from Lungs and Respiratory Health
What is Sick Building Syndrome?
What is the Best Indoor Air Quality Test Kit for a home air check?
^ Top of Page





 1.1
1.1